Wisdom Teeth Removal: Prevent Infection Risks

The process of wisdom teeth removal is a common dental procedure that many individuals undergo, typically between the ages of 17 and 25. This procedure is often necessary due to the potential complications that can arise when wisdom teeth, also known as third molars, do not have enough room to properly emerge and grow in the mouth. Despite its commonality, wisdom teeth removal can lead to infection if not properly managed. Understanding the risks, taking preventive measures, and following post-operative instructions can significantly reduce the likelihood of developing an infection.
Infection Risks Associated with Wisdom Teeth Removal
Infection following wisdom teeth removal can occur due to several factors, including the presence of bacteria in the mouth, the complexity of the procedure, and the patient’s overall health status. Some common signs of infection include increased pain, swelling, redness, fever, and pus or discharge from the extraction site. It’s crucial for patients to be aware of these symptoms and seek immediate medical attention if they experience any of them.
Causes of Infection
- Bacterial Contamination: The mouth is a breeding ground for bacteria, which can easily infect the extraction site if proper care is not taken.
- Dry Socket: This is a common complication where the blood clot that forms over the extraction site is dislodged or does not develop properly, exposing the bone and nerve endings to bacteria and debris.
- Poor Oral Hygiene: Failure to maintain good oral hygiene after the procedure can lead to the accumulation of bacteria and food particles in the extraction site, increasing the risk of infection.
Preventive Measures
Preventing infection after wisdom teeth removal involves a combination of pre-operative, operative, and post-operative measures.
Pre-Operative Measures
- Assess Overall Health: Patients with certain medical conditions or those taking specific medications may need special considerations to minimize infection risk.
- Smoking and Tobacco Cessation: Smoking can significantly impair healing and increase the risk of complications, including infection. Quitting or reducing smoking before and after the procedure is advisable.
- Good Oral Hygiene: Maintaining good oral health before the procedure can reduce the bacterial load in the mouth.
Operative Measures
- Sterilization and Disinfection: Ensuring that all instruments and the surgical site are properly sterilized and disinfected is crucial.
- Antibiotic Prophylaxis: In some cases, especially if there’s a high risk of infection, the dentist or oral surgeon may prescribe antibiotics to be taken before or after the procedure.
Post-Operative Measures
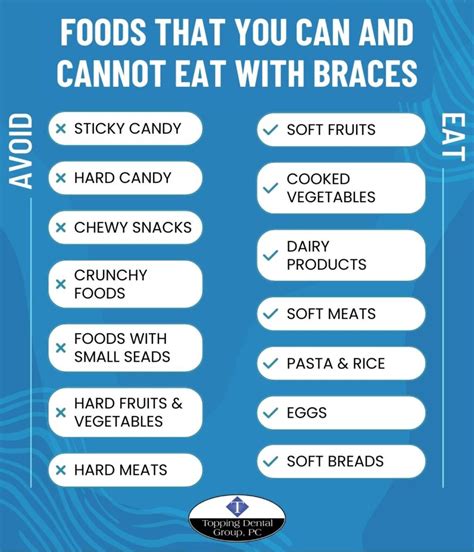
- Follow Instructions: Adhering to the post-operative instructions provided by the dentist or oral surgeon is vital. This includes guidelines on pain management, diet, oral hygiene, and follow-up appointments.
- Maintain Oral Hygiene: Gentle brushing and rinsing with salt water can help keep the extraction site clean without dislodging the blood clot.
- Monitor for Signs of Infection: Being vigilant about signs of infection and seeking medical attention promptly if any concerns arise.
Case Study: Wisdom Teeth Removal and Infection Prevention
A recent case study highlighted the importance of post-operative care in preventing infection after wisdom teeth removal. A 22-year-old male underwent routine wisdom teeth extraction and was instructed on proper post-operative care, including a soft diet, gentle oral hygiene practices, and follow-up appointments. Despite initial discomfort, the patient followed the instructions diligently and attended all scheduled follow-ups. As a result, the healing process was smooth, and there were no signs of infection. This case underscores the significance of patient compliance with post-operative instructions in minimizing the risk of complications.
Decision Framework for Patients
For patients considering wisdom teeth removal, it’s essential to weigh the benefits and risks and make an informed decision. Factors to consider include:
- Necessity of the Procedure: Is the removal necessary due to impacted teeth, crowding, or other complications?
- Risk of Infection: What measures can be taken to minimize this risk, and how will they be implemented?
- Post-Operative Care: What instructions will be followed, and how will compliance be ensured?
Myth vs. Reality: Common Misconceptions About Wisdom Teeth Removal
There are several misconceptions surrounding wisdom teeth removal that can impact a patient’s decision-making process.
Myth: Wisdom teeth always need to be removed.
Reality: Not all wisdom teeth require removal. The decision is based on the specific circumstances of each case, including the position of the teeth, the patient’s overall health, and the presence of any complications.
Myth: Wisdom teeth removal is extremely painful.
Reality: While there may be some discomfort and swelling after the procedure, modern anesthesia and pain management techniques can significantly minimize pain. Most patients can manage post-operative discomfort with over-the-counter pain relievers and by following post-operative instructions.
Technical Breakdown: Understanding the Procedure
Wisdom teeth removal can be performed under local anesthesia, sedation, or general anesthesia, depending on the complexity of the case and the patient’s comfort level. The procedure involves making an incision in the gum tissue to access the tooth, removing any bone that may be covering the tooth, and then extracting the tooth. In some cases, the tooth may need to be sectioned into smaller pieces to facilitate removal.
Future Trends in Wisdom Teeth Removal
Advancements in dental technology and procedures are continuously evolving. One of the emerging trends is the use of laser surgery for wisdom teeth removal, which can potentially reduce healing time and minimize the risk of complications. Additionally, there’s a growing interest in preventive measures, such as early evaluation and intervention, to avoid the need for surgical removal altogether.
Resource Guide: Post-Operative Care
For patients who have undergone wisdom teeth removal, the following resources can be helpful in managing post-operative care:
- Dental Association Websites: Many dental associations provide detailed guidelines on post-operative care, including pain management, diet, and oral hygiene practices.
- Healthcare Provider Instructions: Specific instructions from the dentist or oral surgeon should be followed closely.
- Support Groups: Online forums or support groups can offer valuable advice and reassurance from individuals who have undergone similar procedures.
Conclusion
Wisdom teeth removal is a common procedure that can significantly improve oral health by preventing potential complications associated with impacted or poorly positioned teeth. While there is a risk of infection, understanding the causes, taking preventive measures, and following post-operative instructions can minimize this risk. By being informed and proactive, patients can ensure a smooth recovery and maintain good oral health.
What are the common signs of infection after wisdom teeth removal?
+Common signs of infection include increased pain, swelling, redness, fever, and pus or discharge from the extraction site. If you experience any of these symptoms, it’s essential to seek immediate medical attention.
How can I prevent infection after wisdom teeth removal?
+To prevent infection, follow your dentist or oral surgeon’s post-operative instructions closely. This includes maintaining good oral hygiene, attending follow-up appointments, and being vigilant about signs of infection. Adhering to a soft diet and avoiding smoking can also help in the healing process.
What are the potential complications of wisdom teeth removal?
+Potential complications include dry socket, infection, nerve damage, and prolonged bleeding. However, these complications can be minimized by following post-operative instructions and maintaining good oral health.