Preemie Blood Transfusions Explained: Safety Guide
The decision to administer blood transfusions to premature infants is a complex one, fraught with considerations of both benefit and risk. Premature babies, particularly those born before 32 weeks of gestation, often face significant health challenges, including anemia, low blood pressure, and respiratory distress syndrome. In these critical situations, blood transfusions can be a lifesaving intervention. However, like any medical procedure, blood transfusions come with their own set of risks and potential complications. This comprehensive guide is designed to provide an in-depth exploration of the safety aspects of blood transfusions in preemie care, addressing the underlying principles, indications, benefits, risks, and the future directions in this critical area of neonatal medicine.
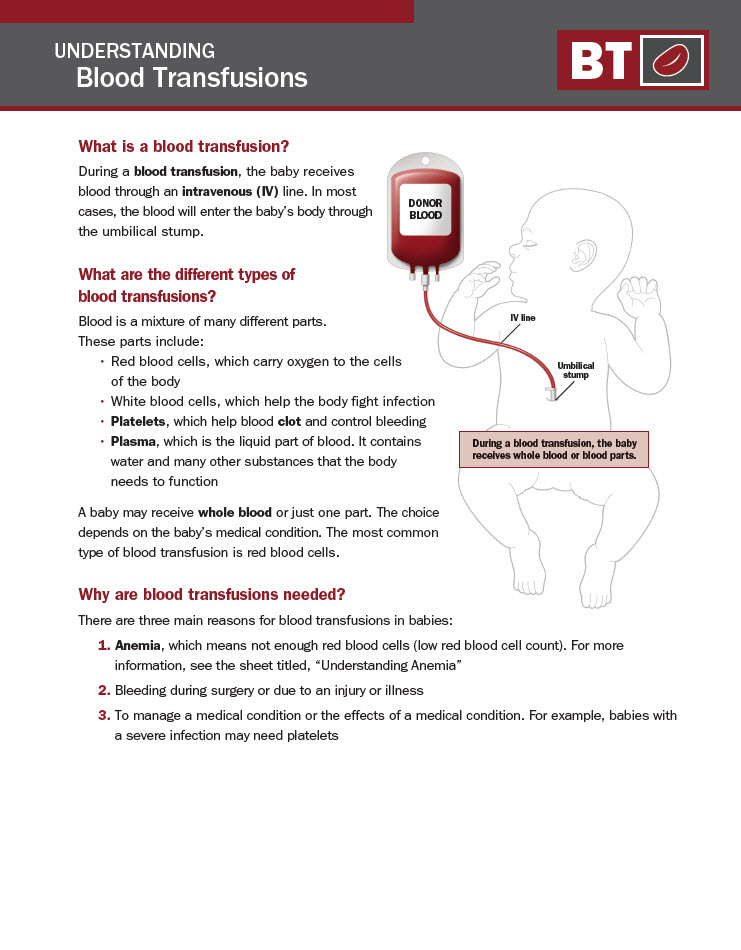
Understanding Blood Transfusions in Preemies
Premature infants, due to their immature organs and systems, may require blood transfusions for a variety of reasons. Anemia, which can result from frequent blood sampling for laboratory tests, is a common indication. Other reasons include low blood volume (hypovolemia), significant blood loss, or the need to increase the red blood cell mass in infants with severe anemia or those undergoing surgery. The blood used for transfusions is carefully screened and matched to minimize the risk of adverse reactions.
The Process of Blood Transfusion
The process of administering a blood transfusion to a premature infant is highly specialized and involves several key steps: 1. Blood Typing and Cross-Matching: Ensuring the blood type of the donor and the recipient are compatible is crucial. This involves both typing the blood (determining if it is A, B, AB, or O) and cross-matching (mixing the donor’s blood with the recipient’s blood to check for any adverse reactions). 2. Selection of Blood Components: Depending on the need, transfusions can involve whole blood, red blood cells, platelets, or fresh frozen plasma. For preemies, red blood cell transfusions are the most common. 3. Administration: The transfused blood is administered through an intravenous line, and the infant is closely monitored for any signs of reaction, such as changes in vital signs, rash, or distress.
Indications for Blood Transfusions
The decision to transfuse a premature infant is based on several factors, including the severity of anemia, the presence of symptomatic anemia (e.g., poor weight gain, tachycardia, or increased need for respiratory support), and the infant’s overall clinical condition. Guidelines suggest considering transfusions when the hemoglobin level falls below a certain threshold, which can vary depending on the gestational age and the infant’s condition.
Benefits of Blood Transfusions
Blood transfusions can significantly improve the clinical condition of premature infants by: - Correcting Anemia: Improving oxygen delivery to tissues, which can enhance growth and development. - Supporting Surgery or Procedures: Allowing for safer surgical interventions by ensuring adequate red blood cell mass. - Managing Blood Loss: Replacing significant blood loss due to surgery, bleeding, or other causes.
Risks and Complications
While potentially lifesaving, blood transfusions carry inherent risks, including: - Transfusion Reactions: Allergic reactions, hemolysis (breakdown of red blood cells), or transfusion-related acute lung injury (TRALI). - Infection: Though rare due to stringent screening, the transmission of infectious agents like viruses or bacteria is a concern. - Immunomodulation: Blood transfusions can affect the immune system, potentially increasing the risk of infections or altering the immune response. - Graft-Versus-Host Disease (GVHD): A rare but potentially fatal complication where immune cells in the transfused blood attack the recipient’s tissues.
Safety Measures and Monitoring
To mitigate these risks, strict safety protocols are in place: - Stringent Blood Screening: Donor blood is carefully tested for infectious agents. - Matching and Typing: Ensuring compatibility reduces the risk of adverse reactions. - Close Monitoring: During and after the transfusion, infants are closely watched for signs of reaction or complications. - Conservative Transfusion Practices: Guidelines encourage the use of the least amount of blood necessary to achieve clinical goals, minimizing exposure to donor blood.
Future Directions
Research continues into optimizing blood transfusion practices for premature infants. Areas of focus include: - Delayed Cord Clamping: Which can reduce the need for early transfusions in preemies. - Autologous Transfusions: Using the infant’s own blood (e.g., from the placenta) to minimize exposure to donor blood. - Erythropoiesis-Stimulating Agents: Medications that stimulate the production of red blood cells, potentially reducing the need for transfusions.
Conclusion
Blood transfusions are a critical component of care for many premature infants, offering a lifesaving intervention for anemia and other conditions. While they come with risks, adherence to strict safety protocols, careful monitoring, and the implementation of evidence-based guidelines minimize these risks. As research progresses, the goal is to further refine transfusion practices, reducing the need for donor blood and enhancing the safety and outcomes for these vulnerable patients.
What are the primary indications for blood transfusions in premature infants?
+The primary indications include severe anemia, significant blood loss, the need to increase red blood cell mass, and support for surgery or medical procedures.
How are blood transfusions administered to premature infants?
+Blood transfusions are administered through an intravenous line, with careful monitoring for any signs of adverse reaction.
What safety measures are in place to minimize the risks associated with blood transfusions in preemies?
+Safety measures include stringent blood screening, careful matching and typing, close monitoring during and after the transfusion, and the use of conservative transfusion practices.