Pancreas Bacteria Diabetes
The human pancreas, a vital organ responsible for producing hormones like insulin and glucagon, has been found to host a unique community of bacteria. Recent research has shed light on the intriguing relationship between the pancreas, its resident bacteria, and the development of diabetes. This complex interplay has significant implications for our understanding of the disease and the potential development of novel therapeutic strategies.
One of the key challenges in studying the pancreatic microbiome is the difficulty in accessing this organ for sampling. However, advancements in technology and methodology have enabled researchers to overcome these hurdles. For instance, a study published in the journal Nature discovered that the pancreas of healthy individuals hosts a diverse range of bacterial species. Interestingly, this diversity is significantly reduced in individuals with type 1 diabetes, suggesting a potential link between the pancreatic microbiome and the development of the disease.
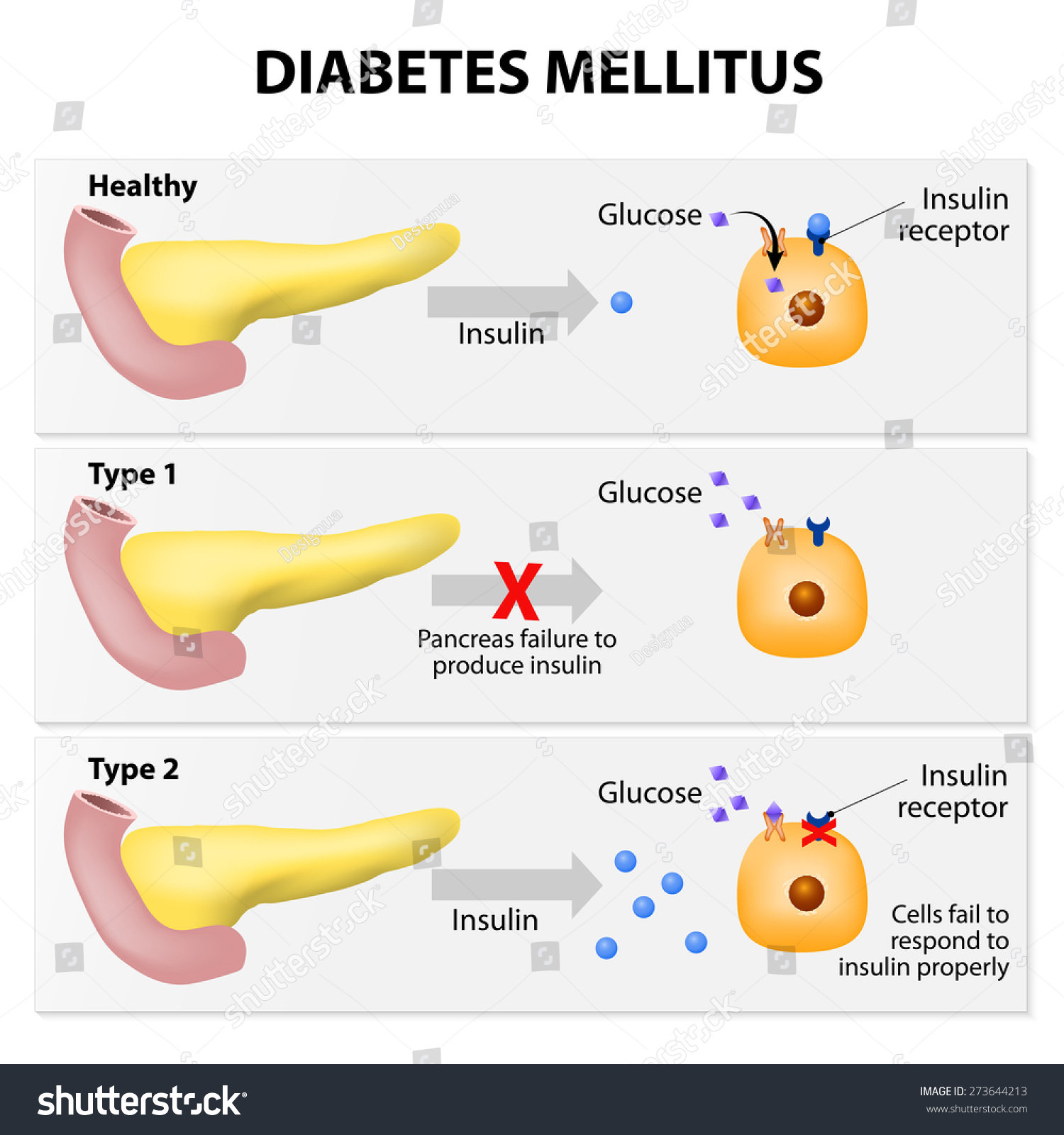
The mechanisms by which pancreatic bacteria might influence diabetes are multifaceted. One theory is that certain bacteria can modulate the immune system, potentially triggering an autoimmune response that destroys insulin-producing beta cells. This is supported by research demonstrating that individuals with type 1 diabetes have higher levels of autoantibodies against pancreatic antigens. Furthermore, the presence of specific bacterial species in the pancreas has been associated with changes in the expression of genes involved in immune regulation and beta-cell function.
In the context of type 2 diabetes, the role of the pancreatic microbiome is equally fascinating. Studies have shown that individuals with type 2 diabetes exhibit alterations in their pancreatic microbiota, characterized by an increased abundance of certain bacterial genera. These changes are thought to contribute to the development of insulin resistance, a hallmark of type 2 diabetes. The exact mechanisms by which this occurs are not fully understood but may involve the production of metabolites that influence glucose metabolism or the modulation of inflammation in the pancreas.
The discovery of a pancreatic microbiome and its potential role in diabetes has opened up new avenues for research and therapeutic intervention. For example, targeting the pancreatic microbiome through the use of probiotics or prebiotics could offer a novel approach to managing or even preventing diabetes. Additionally, understanding how the pancreatic microbiome interacts with the host immune system could lead to the development of immunotherapies designed to preserve beta-cell function.
However, it is crucial to acknowledge the complexity of this field and the need for further research. The pancreatic microbiome is likely influenced by a multitude of factors, including diet, lifestyle, and genetic predisposition. Elucidating the interactions between these factors and the pancreatic microbiome will be essential for developing effective therapeutic strategies.
In terms of practical applications, individuals can take steps to support the health of their pancreatic microbiome. This includes maintaining a balanced diet rich in fiber, which can help support the growth of beneficial bacteria. Additionally, avoiding excessive sugar intake and staying physically active can contribute to a healthy metabolic profile, potentially reducing the risk of developing type 2 diabetes.
Supporting Pancreatic Health
- Maintain a balanced diet rich in fruits, vegetables, and whole grains to support the growth of beneficial bacteria.
- Avoid excessive sugar intake to reduce the risk of metabolic disorders.
- Stay physically active to improve insulin sensitivity and overall metabolic health.
Future research directions should include longitudinal studies to assess how changes in the pancreatic microbiome correlate with the development and progression of diabetes. Additionally, interventional studies evaluating the effects of probiotics, prebiotics, or other microbiome-modulating therapies on diabetes outcomes are urgently needed. The potential for the pancreatic microbiome to serve as a therapeutic target for diabetes management represents an exciting frontier in biomedical research.
What is the relationship between the pancreas and bacteria in diabetes?
+Research has shown that the pancreas hosts a unique community of bacteria, and alterations in this microbiome are associated with the development of diabetes. The exact mechanisms are complex and involve interactions between the bacteria, the immune system, and the pancreas.
Can modifying the pancreatic microbiome help manage or prevent diabetes?
+Targeting the pancreatic microbiome through dietary changes, probiotics, or other interventions may offer a novel approach to managing or preventing diabetes. However, further research is needed to fully understand the therapeutic potential of this approach.
In conclusion, the interplay between the pancreas, its resident bacteria, and diabetes represents a rich area of investigation with significant implications for our understanding and management of the disease. As research continues to unravel the complexities of this relationship, we may uncover new pathways to prevention and treatment, offering hope for the millions of individuals worldwide affected by diabetes.
