Motor Exam Neuro
The motor exam is a crucial component of the neurological examination, providing valuable insights into the functioning of the nervous system. It involves a systematic evaluation of the patient’s motor skills, muscle strength, and reflexes to identify any abnormalities or deficits. In this article, we will delve into the intricacies of the motor exam, exploring its components, techniques, and significance in neurology.
Introduction to the Motor Exam
The motor exam is an essential part of the neurological examination, as it helps healthcare professionals assess the patient’s motor function, coordination, and muscle strength. The exam typically involves a series of tests and evaluations, including muscle strength testing, reflex testing, coordination and balance assessments, and gait evaluation. By analyzing the results of these tests, healthcare professionals can identify potential neurological disorders or injuries affecting the motor system.
Components of the Motor Exam
The motor exam consists of several components, each designed to assess specific aspects of motor function. These components include:
- Muscle Strength Testing: This involves evaluating the patient’s muscle strength by asking them to contract specific muscle groups against resistance. The examiner assesses the patient’s ability to generate force, sustain contractions, and relax muscles.
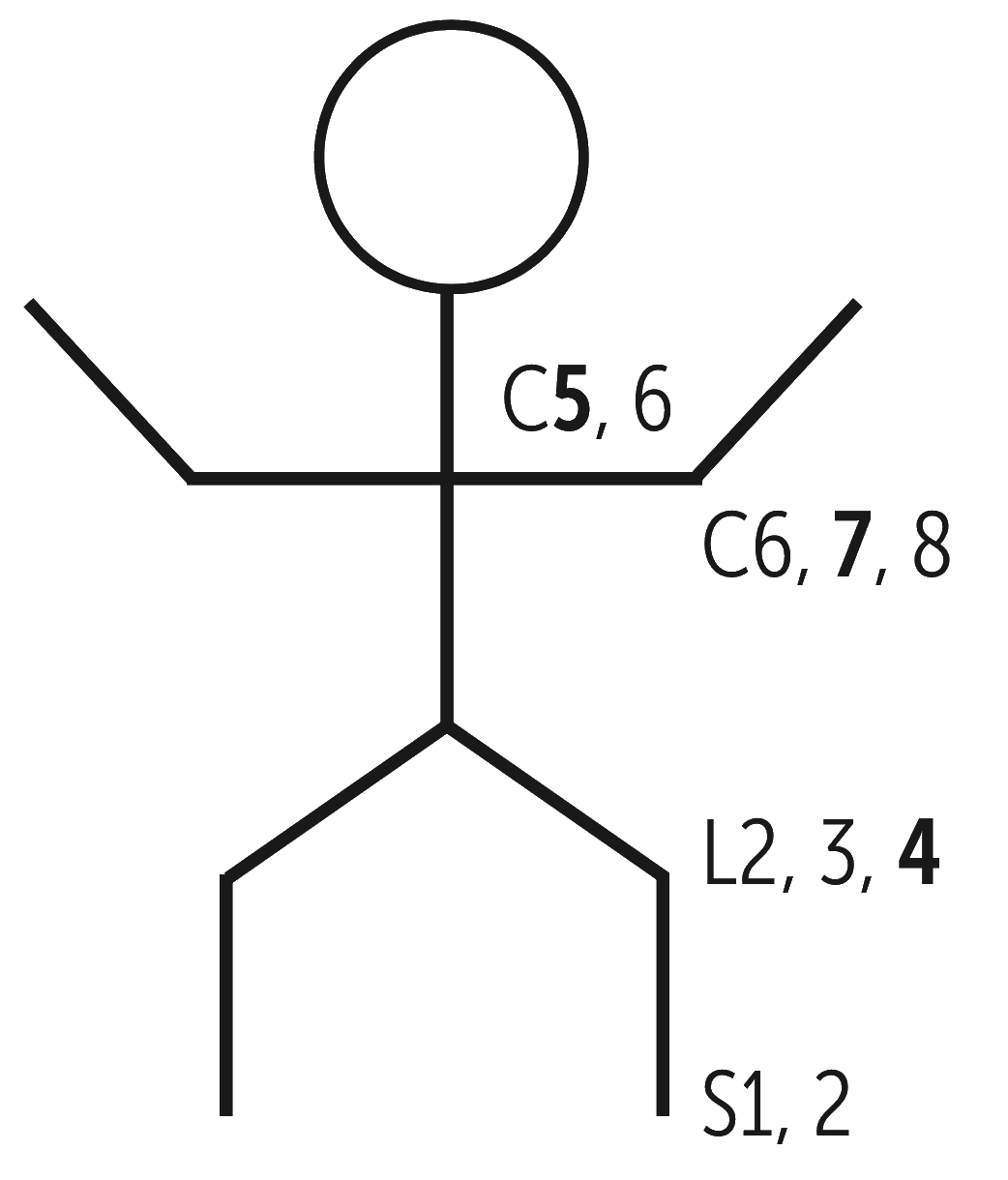
- Reflex Testing: Reflexes are automatic responses to specific stimuli, such as tapping a tendon or stretching a muscle. The examiner evaluates the patient’s reflexes to assess the integrity of the nervous system, particularly the spinal cord and peripheral nerves.
- Coordination and Balance Assessments: These tests evaluate the patient’s ability to perform coordinated movements, such as touching their finger to their nose or walking in a straight line. The examiner assesses the patient’s balance, proprioception (awareness of body position), and fine motor skills.
- Gait Evaluation: The examiner observes the patient’s gait, noting any abnormalities in their walking pattern, such as difficulty initiating steps, shuffling, or stumbling.
Techniques Used in the Motor Exam
Healthcare professionals employ various techniques to perform the motor exam, including:
- Manual Muscle Testing: This involves using the examiner’s hands to apply resistance to specific muscle groups, assessing the patient’s strength and endurance.
- Reflex Hammer: A reflex hammer is used to elicit reflexes by striking specific tendons or muscles.
- Heel-To-Toe Walking: The patient is asked to walk in a straight line, placing the heel of one foot directly in front of the toes of the other foot.
- Finger-to-Nose Testing: The patient is asked to touch their index finger to their nose, then to the examiner’s finger, and back to their nose again, assessing fine motor skills and coordination.
Significance of the Motor Exam in Neurology
The motor exam plays a critical role in neurology, as it helps healthcare professionals:
- Diagnose Neurological Disorders: Abnormalities in the motor exam can indicate conditions such as stroke, spinal cord injury, peripheral neuropathy, or neurodegenerative diseases like Parkinson’s or multiple sclerosis.
- Monitor Disease Progression: Regular motor exams can help healthcare professionals track the progression of neurological disorders, adjusting treatment plans accordingly.
- Assess Treatment Efficacy: The motor exam can be used to evaluate the effectiveness of treatments, such as physical therapy or medication, in improving motor function.
Common Motor Exam Findings
Some common findings in the motor exam include:
- Muscle Weakness: Reduced muscle strength or endurance, which can be indicative of neurological or muscular disorders.
- Reflex Abnormalities: Hyperreflexia (overactive reflexes) or hyporeflexia (underactive reflexes), which can suggest conditions affecting the spinal cord or peripheral nerves.
- Coordination and Balance Deficits: Difficulty with fine motor skills, balance, or coordination, which can indicate cerebellar or vestibular system dysfunction.
- Gait Abnormalities: Abnormalities in walking patterns, such as shuffling or stumbling, which can suggest conditions affecting the basal ganglia or motor control systems.
- Patient fatigue or discomfort, which can affect motor performance
- Normal variability in motor function, which can lead to false positives or false negatives
- Technical difficulties or examiner bias, which can impact the accuracy of the exam
Case Study: Motor Exam in a Patient with Stroke
A 65-year-old patient presents with sudden onset of weakness in their left arm and leg. The motor exam reveals:
- Muscle Weakness: Significant weakness in the left arm and leg, with reduced muscle strength and endurance.
- Reflex Abnormalities: Hyperreflexia in the left arm and leg, suggesting upper motor neuron dysfunction.
- Coordination and Balance Deficits: Difficulty with fine motor skills and balance, indicating cerebellar or vestibular system dysfunction.
- Gait Abnormalities: Hemiplegic gait, with difficulty initiating steps and difficulty with balance.
These findings suggest a diagnosis of stroke, with damage to the motor cortex or descending motor tracts. The patient is referred for further evaluation and treatment, including physical therapy and rehabilitation.
- Obtain a thorough medical history and perform a neurological interview
- Conduct a systematic motor exam, including muscle strength testing, reflex testing, coordination and balance assessments, and gait evaluation
- Use specialized equipment, such as a reflex hammer or manual muscle testing devices, as needed
- Document findings and observations, using standardized scales and scoring systems
- Interpret results in the context of the patient's medical history and other diagnostic findings
Conclusion
The motor exam is a vital component of the neurological examination, providing valuable insights into the functioning of the nervous system. By combining the results of the motor exam with other diagnostic tests, healthcare professionals can develop a comprehensive understanding of the patient’s condition and create effective treatment plans. As we continue to advance our understanding of the motor system and its disorders, the motor exam will remain an essential tool in neurology, helping healthcare professionals diagnose, monitor, and treat a wide range of neurological conditions.
What is the purpose of the motor exam in neurology?
+The motor exam is used to assess the functioning of the nervous system, diagnose neurological disorders, and monitor disease progression.
What are the components of the motor exam?
+The motor exam consists of muscle strength testing, reflex testing, coordination and balance assessments, and gait evaluation.
How is the motor exam used to diagnose neurological disorders?
+The motor exam is used to identify abnormalities in motor function, which can indicate conditions such as stroke, spinal cord injury, or neurodegenerative diseases.
What are some common findings in the motor exam?
+Common findings in the motor exam include muscle weakness, reflex abnormalities, coordination and balance deficits, and gait abnormalities.
How is the motor exam used to monitor disease progression?
+The motor exam is used to track changes in motor function over time, allowing healthcare professionals to adjust treatment plans and monitor the effectiveness of interventions.
