Downward Gaze Palsy
The complexities of human movement and neuroscience are on full display when discussing disorders that affect our ability to control our gaze. One such disorder, though less commonly discussed, is downward gaze palsy, a condition characterized by the inability or significant difficulty in voluntarily moving the eyes downward. This limitation can significantly impact an individual’s daily activities, from reading and using computers to navigating stairs and other everyday environments.
Understanding Downward Gaze Palsy
Downward gaze palsy is often associated with lesions or damage to specific areas of the brainstem, particularly the midbrain, which contains critical circuits for controlling eye movements. The rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF) and the interstitial nucleus of Cajal are two key areas involved in the control of vertical gaze. Damage to these areas, due to stroke, tumor, or degenerative diseases, can lead to impairments in downward gaze.
The presentation of downward gaze palsy can vary, with some individuals experiencing a complete inability to move their eyes downward, while others may have a limited range of motion or require significant effort to achieve downward gaze. In some cases, this condition may be accompanied by other neurological deficits, depending on the underlying cause and the extent of the brain damage.
Causes and Associations
Several conditions and factors can lead to downward gaze palsy, including:
- Stroke and Vascular Diseases: Infarcts in the midbrain can damage the neural pathways responsible for vertical eye movements.
- Tumors: Both benign and malignant tumors in the brainstem can compress or invade the areas critical for eye movement control.
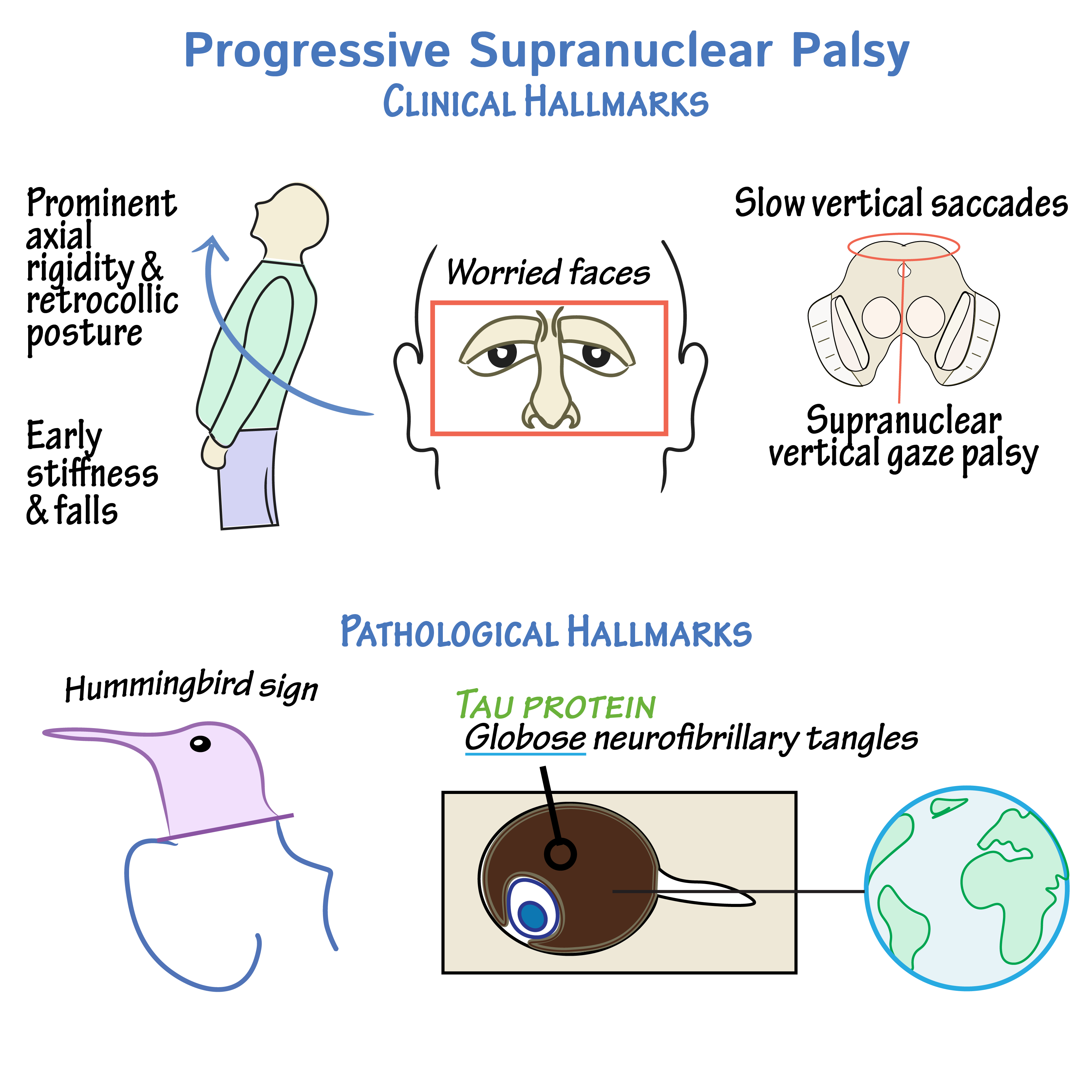
- Degenerative Diseases: Certain neurodegenerative conditions, such as progressive supranuclear palsy (PSP), can lead to downward gaze palsy among other symptoms.
- Traumatic Brain Injury: Severe head trauma can result in damage to the brainstem and subsequent gaze palsy.
- Infections and Inflammatory Conditions: Rarely, infections or inflammatory diseases affecting the brainstem can cause downward gaze palsy.
Diagnosis and Assessment
Diagnosing downward gaze palsy involves a combination of clinical examination, neuroimaging, and sometimes, additional diagnostic tests to identify the underlying cause. Key steps include:
- Clinical Examination: A thorough neurological examination focusing on eye movements, including the assessment of downward gaze.
- Neuroimaging: MRI or CT scans of the brain to identify any structural abnormalities, such as tumors, infarcts, or degenerative changes.
- Electrophysiological Tests: In some cases, tests like electromyography (EMG) of the extraocular muscles or electrooculography (EOG) may be used to further evaluate eye movement control.
Management and Treatment
The management of downward gaze palsy is primarily focused on treating the underlying cause, if possible, and providing supportive care to help manage symptoms and improve quality of life. This may include:
- Pharmacological Interventions: Medications may be used to treat underlying conditions or to manage symptoms.
- Rehabilitation: Physical therapy, occupational therapy, and speech therapy can help individuals adapt to their condition and improve functional abilities.
- Surgical Interventions: In cases where a tumor or other structural lesion is causing the gaze palsy, surgical removal may be considered.
- Compensatory Strategies: Individuals can learn various compensatory strategies, such as using head movements to compensate for limited eye movements, to perform daily tasks more effectively.
Prognosis and Future Directions
The prognosis for individuals with downward gaze palsy varies widely depending on the underlying cause and the extent of the brain damage. In some cases, particularly with acute injuries or conditions, recovery of eye movement may occur. However, in degenerative conditions, the progression of the disease may lead to worsening of symptoms over time.
Ongoing research into the neural control of eye movements and the development of new therapeutic strategies offers hope for improved management and treatment options in the future. Advances in neurophthalmology, neurosurgery, and rehabilitation medicine are critical for enhancing the quality of life for individuals affected by downward gaze palsy and other disorders of eye movement.
What are the common causes of downward gaze palsy?
+Downward gaze palsy can be caused by a variety of conditions including stroke, tumors, degenerative diseases like progressive supranuclear palsy, traumatic brain injury, and infections or inflammatory conditions affecting the brainstem.
How is downward gaze palsy diagnosed?
+Diagnosis involves a clinical examination focusing on eye movements, neuroimaging such as MRI or CT scans to identify structural abnormalities, and sometimes additional tests like electromyography or electrooculography.
What are the treatment options for downward gaze palsy?
+Treatment primarily focuses on addressing the underlying cause, if possible, through pharmacological interventions, rehabilitation, surgical interventions for structural lesions, and teaching compensatory strategies to improve daily functioning.
In conclusion, downward gaze palsy is a complex condition that requires a multidisciplinary approach for diagnosis and management. Understanding its causes, symptoms, and treatment options is crucial for providing the best possible care for individuals affected by this condition. As research continues to unfold the intricacies of the brain and its control over eye movements, there is hope for the development of more effective treatments and improved outcomes for those with downward gaze palsy.

