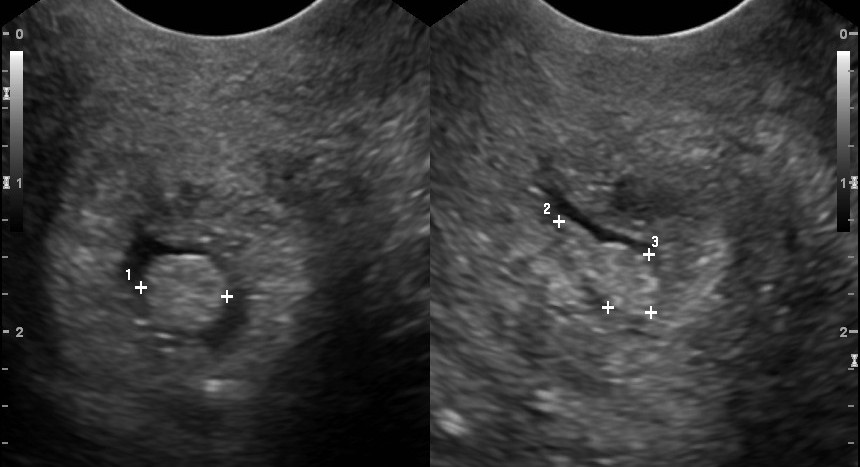
Cervical Polyp Image
When discussing cervical polyps, it’s essential to understand what they are and how they are visually identified. Cervical polyps are growths that occur on the cervical canal, which is the lower part of the uterus in the human female reproductive system. They are usually benign (non-cancerous) but can cause symptoms such as abnormal vaginal bleeding. The diagnosis and understanding of cervical polyps often involve visual identification through medical imaging techniques or direct observation during a pelvic exam.
Visual Appearance
Cervical polyps can vary in size, shape, and color. They are typically described as:
- Small to Large Size: Ranging from a few millimeters to several centimeters in diameter.
- Pedunculated or Sessile: They can be attached to the cervical wall by a stalk (pedunculated) or have a broad base (sessile).
- Red or Pink Color: Due to their rich blood supply, they often appear red or pink.
- Smooth Surface: Usually, the surface of a cervical polyp is smooth, although it can sometimes appear irregular.
Imaging Techniques
While direct visual inspection through colposcopy or during a surgical procedure provides the most straightforward view of cervical polyps, other imaging techniques can also be used for initial diagnosis or to understand the polyp’s relationship with surrounding structures. These include:
- Ultrasound: Can help identify larger polyps and provide information about the polyp’s size and whether it is pedunculated or sessile.
- MRI: Offers detailed images of the uterus and cervix, which can be useful in distinguishing polyps from other types of growths or abnormalities.
- CT Scan: Less commonly used for cervical polyps due to its lower resolution for soft tissue structures compared to ultrasound or MRI but can be part of a broader abdominal or pelvic examination.
Importance of Accurate Diagnosis
Accurate diagnosis of cervical polyps is crucial for determining the appropriate treatment, which often involves removal of the polyp (polypectomy) for symptom relief and to rule out any potential malignancy. The diagnosis process, including visual examination and imaging, helps differentiate cervical polyps from other cervical abnormalities, such as cervicitis or cervical cancer.
Removal and Examination
After removal, a cervical polyp is typically sent for histopathological examination to confirm its nature (benign vs. malignant) and to identify any underlying conditions that may have led to its formation, such as chronic inflammation or hormonal imbalances.
Prevention and Management
While the exact cause of cervical polyps is often not identified, managing factors that might contribute to their development, such as hormonal balance, and ensuring regular gynecological check-ups can help in early detection and treatment.
In conclusion, understanding the visual appearance and characteristics of cervical polyps, along with the use of appropriate imaging techniques, plays a critical role in their diagnosis and management. If you have concerns about cervical polyps or any gynecological issues, consulting a healthcare provider is essential for proper evaluation and care.
What are the common symptoms of cervical polyps?
+Common symptoms include abnormal vaginal bleeding, such as bleeding after intercourse, between menstrual periods, or after menopause. However, many women with cervical polyps do not experience any symptoms.
How are cervical polyps treated?
+Treatment typically involves removal of the polyp, a procedure known as polypectomy, which can often be done in a doctor's office. The removed polyp is then examined to ensure it is not cancerous.
In the context of women’s health, staying informed and proactive about one’s body, including understanding potential issues like cervical polyps, is key to maintaining overall well-being. Regular health check-ups and discussions with healthcare providers can help address any concerns and ensure timely interventions when needed.

