Biofilm Definition Dental
The complex world of biofilms in dental health is a fascinating realm where microscopic organisms thrive, influencing the oral ecosystem in profound ways. At its core, a biofilm is a community of microorganisms that adheres to a surface, embedded in a protective, self-produced matrix of extracellular polymeric substances. This matrix, often composed of polysaccharides, proteins, and DNA, shields the bacteria from environmental stresses, antimicrobial agents, and the host’s immune system, making biofilms a formidable challenge in various medical and dental contexts.
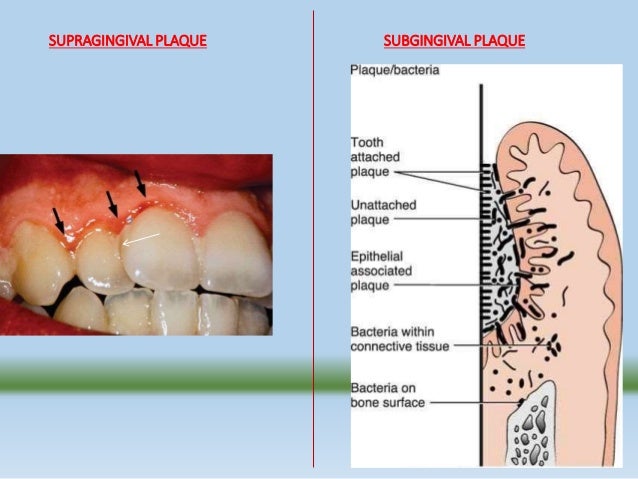
In dentistry, biofilms are notoriously known for their role in the development of dental plaque, a biofilm that forms on the teeth. Dental plaque is a crucial factor in the etiology of dental caries (tooth decay) and periodontal diseases (such as gingivitis and periodontitis), which are among the most prevalent chronic diseases affecting humans worldwide. The bacteria within dental plaque can metabolize dietary sugars and starches to produce acid, which demineralizes tooth enamel and dentin, leading to caries. Additionally, the accumulation of plaque and its associated microbial metabolic products can irritate the gingiva (gums), leading to inflammation and, if left untreated, more severe periodontal disease.
The formation of dental plaque biofilm is a sequential process that involves several stages: 1. Pellicle Formation: The initial step involves the adsorption of salivary proteins and glycoproteins onto the tooth surface, forming the acquired pellicle. This layer modifies the tooth surface, making it more receptive for bacterial adherence. 2. Bacterial Adhesion: The first bacteria to colonize the tooth surface are typically gram-positive, facultatively anaerobic cocci and rods, such as Streptococci. These early colonizers produce adhesive substances that not only help them adhere to the tooth surface but also facilitate the adhesion of other bacteria. 3. Biofilm Maturation: As the biofilm grows, it becomes more complex, with the incorporation of additional bacterial species, including gram-negative, anaerobic bacteria. This diversity leads to a structured community with different metabolic capabilities, further protected by the extracellular matrix. 4. Detachment and Dispersal: Finally, parts of the mature biofilm can detach, dispersing bacteria to other areas of the oral cavity, where they can initiate new biofilm formation.
Understanding the dynamics of dental biofilm formation and its impact on oral health is crucial for the prevention and treatment of dental diseases. Strategies to prevent or control biofilm formation include regular brushing and flossing to remove plaque, the use of antimicrobial mouthwashes, and professional dental cleanings. Furthermore, dietary habits, such as limiting sugary and starchy foods, play a significant role in reducing the risk of dental caries and other biofilm-related diseases.
In recent years, research has focused on developing more effective methods to combat dental biofilms, including the use of novel antimicrobial agents, probiotics, and devices that can disrupt or prevent biofilm formation. For instance, certain mouthwashes contain ingredients like triclosan or chlorhexidine, which have been shown to inhibit bacterial growth and biofilm formation. Additionally, there is growing interest in the potential of nanotechnology and photodynamic therapy as innovative approaches to managing dental biofilms.
What is the main cause of dental plaque formation?
+The main cause of dental plaque formation is the adhesion of bacteria to the tooth surface, facilitated by the acquired pellicle and the production of adhesive substances by early colonizing bacteria.
How can dental biofilms be prevented or controlled?
+Dental biofilms can be prevented or controlled through good oral hygiene practices such as regular brushing and flossing, use of antimicrobial mouthwashes, professional dental cleanings, and limiting dietary sugars and starches.
What are some emerging strategies for managing dental biofilms?
+Emerging strategies include the use of novel antimicrobial agents, probiotics, nanotechnology, and photodynamic therapy to disrupt or prevent biofilm formation.
In conclusion, dental biofilms are complex microbial communities that play a significant role in oral health and disease. Understanding their formation, structure, and impact is essential for developing effective prevention and treatment strategies. As research continues to unravel the intricacies of biofilm biology, new and innovative approaches to managing these resilient microbial communities are being explored, offering promising avenues for improving oral health outcomes.
