Air Bubble In Subcutaneous Injection
The administration of subcutaneous injections is a common practice in medical settings for the delivery of various medications, including insulin, vaccines, and other therapeutic agents. Despite its widespread use, one issue that can arise during the administration of these injections is the formation of an air bubble within the injected substance. This phenomenon is particularly relevant when considering the impact of air bubbles in subcutaneous injections, as it can affect the efficacy, safety, and patient comfort associated with the treatment.
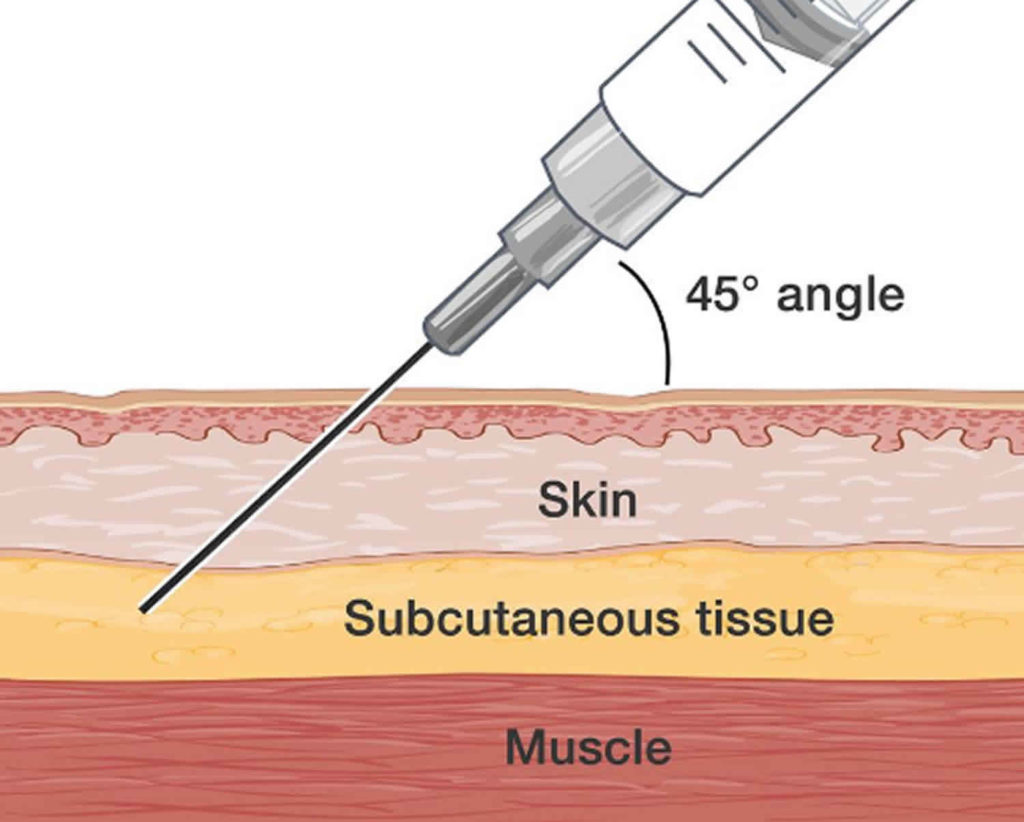
To understand the implications of air bubbles in subcutaneous injections, it’s essential to first grasp the basics of how these injections are administered and the importance of proper technique. Subcutaneous injections are given into the fatty tissue just beneath the skin, rather than into a muscle or vein. This method allows for the slow absorption of medication into the bloodstream, providing a sustained release of the therapeutic agent. However, the introduction of air into the subcutaneous tissue during injection can lead to complications.
Causes of Air Bubbles in Subcutaneous Injections
Several factors contribute to the formation of air bubbles during subcutaneous injections. One of the primary causes is the technique used by the healthcare provider. If the needle is not inserted correctly or if the plunger is pushed too quickly, it can create a vacuum effect that pulls air into the syringe or the injection site. Additionally, not removing air bubbles from the syringe before injection can also lead to this issue. Furthermore, the type of medication and its viscosity can influence the likelihood of air bubble formation; thicker substances might be more prone to trapping air bubbles.
Consequences of Air Bubbles
The presence of air bubbles in subcutaneous injections can have several consequences, ranging from minor discomfort to more serious complications. One of the most immediate effects is pain at the injection site, which can be exacerbated by the air bubble. In some cases, the body may react to the foreign substance (air) by forming a local inflammatory response, leading to redness, swelling, and further discomfort. More significantly, if a large air bubble is introduced, it could potentially lead to a condition known as subcutaneous emphysema, where air gets trapped in the tissues, causing swelling and potentially affecting the function of surrounding tissues.
Prevention and Management
Preventing the formation of air bubbles in subcutaneous injections is easier than managing the consequences after they occur. Healthcare providers can take several precautions to minimize the risk. Before administering the injection, they should ensure that all air is removed from the syringe by gently tapping it and pressing the plunger until a small amount of medication is released. This step helps to eliminate any air that might have been introduced during the preparation of the dose. Furthermore, using the correct injection technique, including inserting the needle at the right angle and pushing the plunger slowly, can reduce the likelihood of creating a vacuum effect that pulls air into the tissue.
If an air bubble does form, management strategies depend on the severity of the reaction. In most cases, minor reactions such as local pain or redness can be managed with over-the-counter pain relievers or topical creams to reduce inflammation. However, if more serious complications arise, such as significant swelling or signs of infection, medical attention is necessary. In rare cases, intervention might be required to remove the trapped air or to treat any secondary infections.
Best Practices for Healthcare Providers
Healthcare providers play a crucial role in preventing air bubbles in subcutaneous injections. Training in proper injection technique, including how to handle the syringe, remove air bubbles, and administer the medication slowly, is essential. Regular review of guidelines and updates on best practices can also help in minimizing the occurrence of air bubbles. Moreover, patient education on what to expect during and after an injection, as well as how to report any adverse effects, can improve outcomes and patient satisfaction.
Future Directions
The development of new technologies and techniques in the administration of subcutaneous injections is ongoing. Innovations such as auto-injectors and prefilled syringes are designed to make the process simpler and less prone to errors, including the formation of air bubbles. Additionally, research into the physical properties of medications and how they interact with the body’s tissues during injection can provide valuable insights into minimizing complications.
FAQs
What are the most common causes of air bubbles in subcutaneous injections?
+The most common causes include improper injection technique, failure to remove air from the syringe before injection, and the physical properties of the medication itself.
How can healthcare providers prevent air bubbles during subcutaneous injections?
+Prevention includes ensuring all air is removed from the syringe, using the correct injection angle, and administering the medication slowly to avoid creating a vacuum effect.
What are the potential complications of air bubbles in subcutaneous injections?
+Potential complications include pain at the injection site, local inflammatory response, and in rare cases, subcutaneous emphysema. Severe reactions may require medical intervention.
In conclusion, while air bubbles in subcutaneous injections are a potential complication, they can largely be prevented through proper technique, patient education, and the use of advanced technologies designed to simplify and improve the injection process. As medical practices continue to evolve, the focus on minimizing errors and enhancing patient safety will remain paramount. By understanding the causes, consequences, and best practices for preventing air bubbles, healthcare providers can offer higher quality care and improve patient outcomes.
